Antenatal Depression and Its Risk Factors Among Public Clinic Attendees
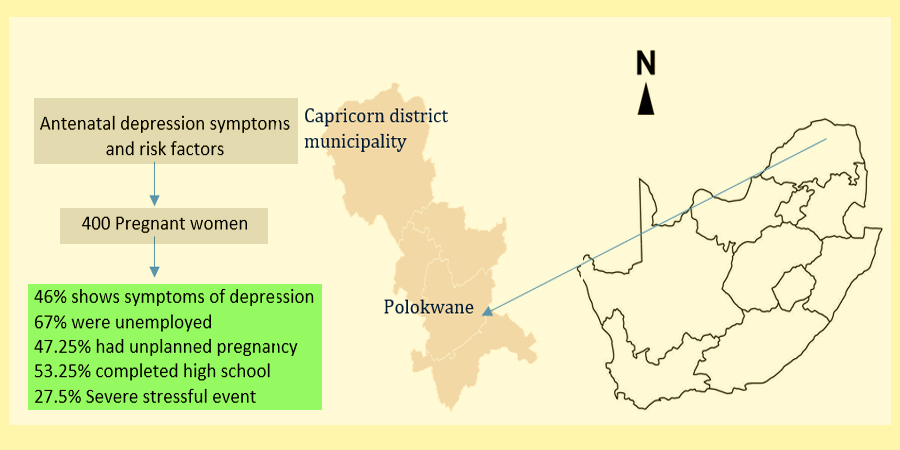
A Cross-Sectional Study in Urban and Rural Area of Limpopo, South Africa
DOI:
https://doi.org/10.24252/al-sihah.v17i1.51825Keywords:
prevalence; maternal depression; antenatal depression symptoms; Edinburgh postnatal depression scale; screening; primary health care facilities; South Africa.Abstract
Antenatal depression is a common yet underdiagnosed mental health issue with serious implications for maternal and child well-being. While its prevalence is well-documented globally, limited research exists on its burden and contributing factors within primary health care settings in rural South Africa. The purpose of this study was to screen for symptoms of antenatal depression and explore associated factors among clinic attendees in primary health care facilities in the Capricorn Health District, Limpopo Province, South Africa. The Edinburgh Postnatal Depression Scale-10 (EPDS-10) was used to screen for symptoms of antenatal depression, and a quantitative questionnaire was used to collect socio-demographic data. The ages of the sample ranged from 18 to 44 years, with a mean age of 28 years. The greatest proportion, 46% (n = 186), were single, and the majority were unemployed, 67% (n = 270), with 53.25% (n = 243) having completed high school. Almost half, 47.25% (n = 189), had not planned their pregnancy. The prevalence of antenatal depression symptoms was high, at 46% (n = 184). Factors associated with antenatal depression symptoms included being unemployed, having a previous diagnosis of postnatal depression (PND), dissatisfaction with the relationship with one’s partner, and lack of financial, social, and emotional support from the partner, as well as experiencing severe stress in the previous six weeks. The results highlight the need for routine antenatal screening for depression in primary health care facilities, where the majority of pregnant women access prenatal care.
Downloads
References
Afeworki, R., Smits, J., Tolboom, J., & van der Ven, A. (2015). Positive effect of large birth intervals on early childhood hemoglobin levels in Africa is limited to girls: cross-sectional DHS study. PLoS ONE, 10(6), 1–14. https://doi.org/10.1371/journal.pone.0131897
Abrahams, J. M., & Stellenberg, E. L. (2015). Prevalence of and factors influencing postnatal depression in a rural community in South Africa. African Journal of Primary Health Care and Family Medicine, 7(1), 1-8. http://dx.doi.org/10.4102/phcfm.v7i1.874
Bedaso, A., Adams, J., Peng, W., & Sibbritt, D. (2021). The association between social support and antenatal depressive and anxiety symptoms among Australian women. BMC pregnancy and childbirth, 21, 1-12. https://doi.org/10.1186/s12884-021-04188-4
Biaggi, A., Conroy, S., Pawlby, S. and Pariante, C.M., 2016. Identifying the women at risk of antenatal anxiety and depression: A systematic review. Journal of affective disorders, 191, pp.62-77. https://doi.org/10.1016/j.jad.2015.11.014
Biratu, A., & Haile, D. (2015). Prevalence of antenatal depression and associated factors among pregnant women in Addis Ababa, Ethiopia: a cross-sectional study. Reproductive health, 12, 1-8. https://doi.org/10.1186/s12978-015-0092-x
Brittain, K., Myer, L., Koen, N., Koopowitz, S., Donald, K. A., Barnett, W., & Stein, D. J. (2015). Risk factors for antenatal depression and associations with infant birth outcomes: results from a S outh a frican birth cohort study. Paediatric and perinatal epidemiology, 29(6), 505-514. https://doi.org/10.1111/ppe.12216
Brown, S., & Sprague, C. (2021). Health care providers’ perceptions of barriers to perinatal mental healthcare in South Africa. BMC Public Health, 21, 1-13. https://doi.org/10.1186/s12889-021-11954-8
Cena, L., Mirabella, F., Palumbo, G., Gigantesco, A., Trainini, A., & Stefana, A. (2021). Prevalence of maternal antenatal and postnatal depression and their association with sociodemographic and socioeconomic factors: A multicentre study in Italy. Journal of Affective Disorders, 279, 217-221. https://doi.org/10.1016/j.jad.2020.09.136
Christodoulou, J., Le Roux, K., Tomlinson, M., Le Roux, I. M., Katzen, L. S., & Rotheram-Borus, M. J. (2019). Perinatal maternal depression in rural South Africa: Child outcomes over the first two years. Journal of affective disorders, 247, 168-174. https://doi.org/10.1016/j.jad.2019.01.019
Coll, C.D.V.N., da Silveira, M.F., Bassani, D.G., Netsi, E., Wehrmeister, F.C., Barros, F.C. and Stein, A., 2017. Antenatal depressive symptoms among pregnant women: Evidence from a Southern Brazilian population-based cohort study. Journal of Affective Disorders, 209, pp.140-146. https://doi.org/10.1016/j.jad.2016.11.031
Curry, S. J., Krist, A. H., Owens, D. K., Barry, M. J., Caughey, A. B., Davidson, K. W., & US Preventive Services Task Force. (2019). Interventions to prevent perinatal depression: US Preventive Services Task Force recommendation statement. Jama, 321(6), 580-587. https://doi:10.1001/jama.2019.0007
Dadi, A. F., Wolde, H. F., Baraki, A. G., & Akalu, T. Y. (2020). Epidemiology of antenatal depression in Africa: a systematic review and meta-analysis. BMC pregnancy and childbirth, 20, 1-13. https://doi.org/10.1186/s12884-020-02929-5
Dadi, A.F., Miller, E.R., Bisetegn, T.A. and Mwanri, L., 2020. Global burden of antenatal depression and its association with adverse birth outcomes: an umbrella review. BMC public health, 20, pp.1-16. https://doi.org/10.1186/s12889-020-8293-9
Dagher, R. K., Bruckheim, H. E., Colpe, L. J., Edwards, E., & White, D. B. (2021). Perinatal depression: Challenges and opportunities. Journal of Women's Health, 30(2), 154-159. https://doi.org/10.1089/jwh.2020.8862
Dibaba, Y., Fantahun, M., & Hindin, M. J. (2013). The association of unwanted pregnancy and social support with depressive symptoms in pregnancy: evidence from rural Southwestern Ethiopia. BMC pregnancy and childbirth, 13, 1-8. https://doi.org/10.1186/1471-2393-13-135
Eastwood, J., Ogbo, F. A., Hendry, A., Noble, J., Page, A., & Early Years Research Group (EYRG). (2017). The impact of antenatal depression on perinatal outcomes in Australian women. PLoS One, 12(1), e0169907. https://doi.org/10.1371/journal.pone.0169907
Getinet, W., Amare, T., Boru, B., Shumet, S., Worku, W., & Azale, T. (2018). Prevalence and risk factors for antenatal depression in Ethiopia: systematic review. Depression research and treatment, 2018(1), 3649269. https://doi.org/10.1155/2018/3649269
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Mulalo Salane, Kebogile Mokwena

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.