Sexually Transmitted Infections among Adolescents in Greater Letaba, South Africa
Prevalence and Gender-Specific Risk Factors
DOI:
https://doi.org/10.24252/diversity.v6i1.56699Keywords:
hiv testing, patient discharge, prevalence, sexually transmitted diseases, south africaAbstract
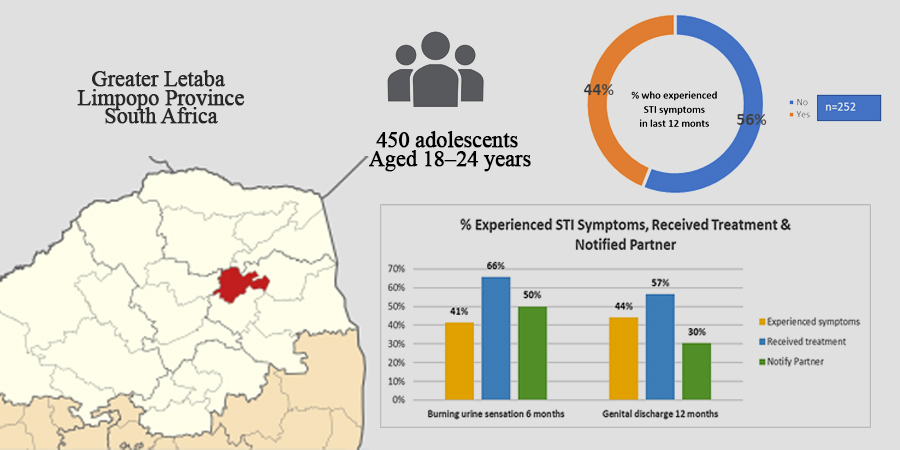
Adolescents remain highly vulnerable to sexually transmitted infections (STIs) due to behavioral, biological, and socio-cultural determinants, yet there is limited evidence from rural sub-Saharan Africa addressing the prevalence and gender-specific patterns of risk. This study aimed to determine the prevalence of STIs and associated risk factors among adolescents in the Greater Letaba sub-district of Limpopo Province, South Africa. A quantitative, descriptive, cross-sectional survey was conducted among 450 participants aged 18–24 years. Data on socio-demographics, sexual practices, STI-related symptoms, and health-seeking behaviors were collected and analyzed. The results showed that 44% of respondents reported STI-related symptoms within the past year, with genital discharge (44%) and dysuria (41%) being the most common. Male participants exhibited significantly higher engagement in risky sexual behaviors, including transactional sex, multiple or non-regular partners, and alcohol use during last intercourse (p<0.001). Males also demonstrated higher rates of condom use, negotiation confidence, and HIV testing uptake compared to females, who expressed greater willingness to test with a partner. The findings underscore the dual challenge of high-risk sexual practices and gendered disparities in STI prevention, suggesting the importance of targeted, gender-sensitive interventions. Integrating Islamic values of modesty, mutual responsibility, and protection of health can strengthen preventive strategies, aligning with the Sustainable Development Goals to improve adolescent and family health outcomes.
Downloads
References
Achen, S., Atekyereza, P., & Rwabukwali, C. B. (2021). The role of culture in influencing sexual and reproductive health of pastoral adolescent girls in Karamoja sub-region in Uganda. Pastoralism, 11(1). https://doi.org/10.1186/s13570-020-00188-9
Adeniyi, O. V., Nwogwugwu, C., Ajayi, A. I., & Lambert, J. (2021). Barriers to and facilitators of HIV serostatus disclosure to sexual partners among postpartum women living with HIV in South Africa. BMC public health, 21(1), 915. https://doi.org/10.1186/s12889-021-10955-x
Alageel, S., Alsadhan, N. M., Alkhaldi, G., Alkasabi, R., & Alomair, N. (2024). Public perceptions of HIV/AIDS awareness in the Gulf Council Cooperation countries: a qualitative study. International Journal for Equity in Health, 23(1), 269. https://doi.org/10.1186/s12939-024-02346-6
Alekhya, G., Parida, S. P., Giri, P. P., Begum, J., Patra, S., & Sahu, D. P. (2023). Effectiveness of school-based sexual and reproductive health education among adolescent girls in Urban areas of Odisha, India: a cluster randomized trial. Reproductive Health, 20(1), 105. https://doi.org/10.1186/s12978-023-01643-7
AlJahsh, M. A. I. (2024). Science and Islamic ethics: Navigating artificial womb technology through Quranic principles. Heliyon, 10(17). https://doi.org/10.1016/j.heliyon.2024.e36793
Appiah, C. K., Dowou, R. K., Balame, S. K., Adzigbli, L. A., Yeboah, P. A., Aboagye, R. G., & Cadri, A. (2023). Self-reported sexually transmitted infections among adolescent girls and young women in Mali: analysis of prevalence and predictors. BMJ open, 13(4), e069226. https://doi.org/10.1136/bmjopen-2022-069226
Ayerdi Aguirrebengoa, O., Vera Garcia, M., Rueda Sanchez, M., D´Elia, G., Chavero Méndez, B., Alvargonzalez Arrancudiaga, M., Bello León, S., Puerta López, T., Clavo Escribano, P., Ballesteros Martín, J., Menendez Prieto, B., Fuentes, M. E., García Lotero, M., Raposo Utrilla, M., Rodríguez Martín, C., & Del Romero Guerrero, J. (2020). Risk factors associated with sexually transmitted infections and HIV among adolescents in a reference clinic in Madrid. PLOS ONE, 15(3), e0228998. https://doi.org/10.1371/journal.pone.0228998
Ayodele, A., Isiaka, M., & Nasirudeen, I. A. (2025). 'I Offered What I Have for What I Want’: A Study of Transactional Hook-Up Practices by Young Females in Nigeria: A. Ayodele et al. Sexuality & Culture, 1-36. https://doi.org/10.1007/s12119-025-10422-4
Boyd, J., Sexton, O., Angus, C., Meier, P., Purshouse, R. C., & Holmes, J. (2022). Causal mechanisms proposed for the alcohol harm paradox—a systematic review. Addiction, 117(1), 33-56. https://doi.org/10.1111/add.15567
Cain, D., Salsabilian, B., Jones, S. S., & Starks, T. J. (2023). Substance use, sexual agreements, and sexual risk behaviors among adolescent sexual minority males (aged 13–17) in the United States. Journal of Adolescent Health, 73(4), 746-752. https://doi.org/10.1016/j.jadohealth.2023.05.032
Carels, C., Florence, M., Adams, S., Sinclair, D. L., & Savahl, S. (2022). Youths’ perceptions of the relation between alcohol consumption and risky sexual behaviour in the Western Cape, South Africa: a qualitative study. Child indicators research, 15(4), 1269-1293. https://doi.org/10.1007/s12187-022-09913-9
Centers for Disease Control and Prevention. (2023). Sexually transmitted infections prevalence in the United States. www.cdc.gov
Cho, H. S., & Yang, Y. (2023). Relationship between alcohol consumption and risky sexual behaviors among adolescents and young adults: A meta-analysis. International Journal of Public Health, 68, 1605669. https://doi.org/10.3389/ijph.2023.1605669
Dadzie, L. K., Agbaglo, E., Okyere, J., Aboagye, R. G., Arthur-Holmes, F., Seidu, A. A., & Ahinkorah, B. O. (2022). Self-reported sexually transmitted infections among adolescent girls and young women in sub-Saharan Africa. International Health, 14(6), 545-553. https://doi.org/10.1093/inthealth/ihab088
Damian, J. U., Hlungwane, E., & Tshitangano, T. G. (2024). Barriers and Mythical Practices of Teenagers Regarding the Prevention of Sexually Transmitted Infections in Rural Areas of Limpopo Province, South Africa. Healthcare, 12(3), 355. https://doi.org/10.3390/healthcare12030355
Damian, J. U., Hlungwane, E., & Tshitangano, T. G. (2024). Barriers and Mythical Practices of Teenagers Regarding the Prevention of Sexually Transmitted Infections in Rural Areas of Limpopo Province, South Africa. Healthcare, 12(3), 355. https://doi.org/10.3390/healthcare12030355
Francis, S. C., Mthiyane, T. N., Baisley, K., Mchunu, S. L., Ferguson, J. B., Smit, T., Crucitti, T., Gareta, D., Dlamini, S., Mutevedzi, T., Seeley, J., Pillay, D., McGrath, N., & Shahmanesh, M. (2018). Prevalence of sexually transmitted infections among young people in South Africa: A nested survey in a health and demographic surveillance site. PLOS Medicine, 15(2), e1002512. https://doi.org/10.1371/journal.pmed.1002512
Karim, S. S. A., & Baxter, C. (2021). HIV incidence trends in Africa: young women at highest risk. The Lancet HIV, 8(7), e389-e390. https://doi.org/10.1016/s2352-3018(21)00079-5
Kahn, L. S., Wozniak, M. L., Doscher, T., Moore, C., & Vest, B. M. (2022). Treatment experiences among people who use opioids: A social ecological approach. Qualitative Health Research, 32(8-9), 1386-1398. https://doi.org/10.1177/10497323221104315
Lin, C. L., Ye, Y., Lin, P., Lai, X. L., Jin, Y. Q., Wang, X., & Su, Y. S. (2021). Safe Sexual Behavior Intentions among College Students: The Construction of an Extended Theory of Planned Behavior. International Journal of Environmental Research and Public Health, 18(12), 6349. https://doi.org/10.3390/ijerph18126349
Llangarí-Arizo, L. M., Broad, C. E., Zhou, L., Mateo, M. M., Moreno, C. I., Cevallos, M. M., & Sadiq, S. T. (2024). Sexually transmitted infections among at-risk women in Ecuador: implications for global prevalence and testing practices for STIs detected only at the anorectum in female sex workers. Sexually Transmitted Infections, 100(8), 504-511. https://doi.org/10.1136/sextrans-2023-056075
Magezi, V., Hoffman, J., & Leeson, G. W. (2025). Understanding Church-Led Adolescent and Youth Sexual Reproductive Health (AYSRH) Interventions Within the Framework of Church Beliefs and Practices in South Africa: A Qualitative Study. Healthcare, 13(8), 907. https://doi.org/10.3390/healthcare13080907
Mbizvo, M. T., Kasonda, K., Muntalima, N. C., Rosen, J. G., Inambwae, S., Namukonda, E. S., Mungoni, R., Okpara, N., Phiri, C., Chelwa, N., & Kangale, C. (2023). Comprehensive sexuality education linked to sexual and reproductive health services reduces early and unintended pregnancies among in-school adolescent girls in Zambia. BMC Public Health, 23(1). https://doi.org/10.1186/s12889-023-15023-0
McBride, B., Shannon, K., Strathdee, S., & Goldenberg, S. M. (2021). Structural determinants of HIV/STI prevalence, HIV/STI/SRH access, and condom use among immigrant sex workers globally: a systematic review. AIDS (London, England), 35(9), 1461. https://doi.org/10.1097/QAD.0000000000002910
Michaelson, V., Pilato, K. A., & Davison, C. M. (2021). Family as a health promotion setting: A scoping review of conceptual models of the health-promoting family. PLOS ONE, 16(4), e0249707. https://doi.org/10.1371/journal.pone.0249707
Morales, A., Espada, J. P., Orgilés, M., Escribano, S., Johnson, B. T., & Lightfoot, M. (2018). Interventions to reduce risk for sexually transmitted infections in adolescents: A meta-analysis of trials, 2008-2016. PLOS ONE, 13(6), e0199421. https://doi.org/10.1371/journal.pone.0199421
Scheinfeld, E. (2023). The Role of Shame, Stigma, and Family Communication Patterns in the Decision to Disclose STIs to Parents in Order to Seek Support. International Journal of Environmental Research and Public Health, 20(6), 4742. https://doi.org/10.3390/ijerph20064742
Seidu, A. A., Aboagye, R. G., Okyere, J., Agbemavi, W., Akpeke, M., Budu, E., Saah, F. I., Tackie, V., & Ahinkorah, B. O. (2021). Women’s autonomy in household decision-making and safer sex negotiation in sub-Saharan Africa: An analysis of data from 27 Demographic and Health Surveys. SSM-Population Health, 14, 100773. https://doi.org/10.1016/j.ssmph.2021.100773
Shangase, N., Kharsany, A. B. M., Ntombela, N. P., Pettifor, A., & McKinnon, L. R. (2021). A Systematic Review of Randomized Controlled Trials of School Based Interventions on Sexual Risk Behaviors and Sexually Transmitted Infections Among Young Adolescents in Sub-Saharan Africa. AIDS and Behavior, 25(11), 3669–3686. https://doi.org/10.1007/s10461-021-03242-8
Stavitz, J. (2024). Understanding micronutrient access through the lens of the social ecological model: exploring the influence of socioeconomic Factors—A qualitative exploration. Nutrients, 16(11), 1757. https://doi.org/10.3390/nu16111757
Wang, X., Jin, Y., Tian, M., Zhuo, Q., Lin, C. L., Hu, P., & Wang, T. (2022). Safe-sex behavioral intention of Chinese college students: examining the effect of sexual knowledge using the theory of planned behavior. Frontiers in Psychology, 13, 805371. https://doi.org/10.3389/fpsyg.2022.805371
Wiafe, S., Mihan, A., & Davison, C. M. (2021). Neighborhood-level influences and adolescent health risk behaviors in rural and urban Sub-Saharan Africa: A systematic review. International journal of environmental research and public health, 18(14), 7637. https://doi.org/10.3390/ijerph18147637
Woldesenbet, S., Kufa, T., Lombard, C., Manda, S., Morof, D., Cheyip, M., Ayalew, K., & Puren, A. (2021). The prevalence of unintended pregnancy and its association with HIV status among pregnant women in South Africa, a national antenatal survey, 2019. Scientific Reports, 11(1). https://doi.org/10.1038/s41598-021-03096-z
World Health Organization. (2023). Sexually transmitted infections among adolescents: The need for adequate health services. www.who.int
Zhang, Y., Guy, R., Camara, H., Applegate, T. L., Wiseman, V., Treloar, C., & Lafferty, L. (2022). Barriers and facilitators to HIV and syphilis rapid diagnostic testing in antenatal care settings in low-income and middle-income countries: a systematic review. BMJ Global Health, 7(11), e009408. https://doi.org/10.1136/bmjgh-2022-009408
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Maite Leinett Thobakgale, Mathildah Mpata Mokgatle, Atholl Klienhans, Muhammad Hoque

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.




