Prevalence of Depression and Anxiety Symptoms in A Sample of Christian Denominations
A Study From South Africa
DOI:
https://doi.org/10.24252/diversity.v6i1.58862Keywords:
anxiety, depression, screening, faith-based, South AfricaAbstract
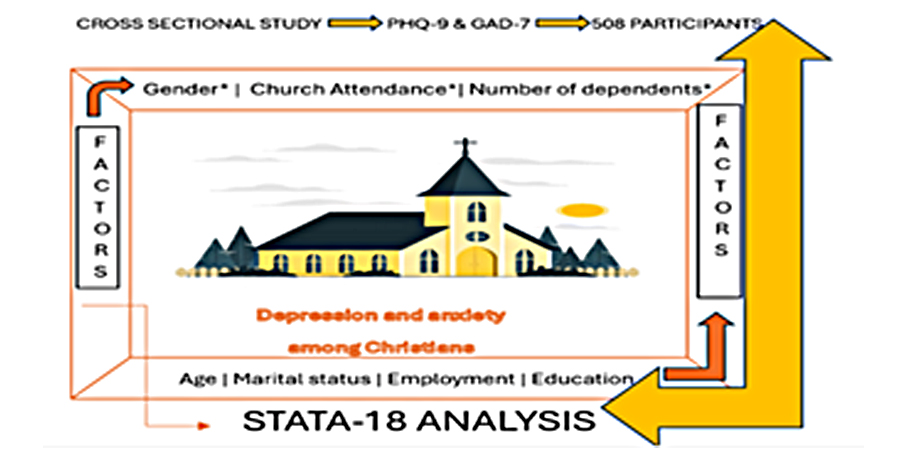
The rising global prevalence of mental disorders, particularly depression and anxiety, underscores the urgent need to assess their burden within communities. Faith-based groups represent a unique population for such assessments as they include diverse segments of society while also functioning as significant social and spiritual support systems. This study aimed to determine the prevalence of depressive and anxiety symptoms among members of Christian denominations in South Africa. A quantitative cross-sectional survey was conducted across various provinces, and data were collected using the Patient Health Questionnaire (PHQ-9) and the Generalized Anxiety Disorder Scale (GAD-7). A total of 508 participants constituted the final sample. The findings revealed a prevalence of 40.94% for depression and 38.98% for anxiety symptoms. Inferential analysis indicated significant associations between gender, number of dependents, and frequency of church attendance with both depression and anxiety symptoms (p≤0.05). These results highlight the elevated burden of mental health symptoms within faith-based populations, exceeding previously reported rates in the general population. The findings emphasize the importance of integrating mental health awareness and support into church settings to reduce stigma, provide targeted interventions, and promote family and community well-being within South Africa.
Downloads
References
Ademiluka, S. (2021). Marriage as a choice or duty: Considering Nigerian Christians’ attitude to singlehood from the biblical perspective. In Die Skriflig, 58(1). https://doi.org/10.4102/ids.v55i1.2674
Ahmad, M. S., Shah, R., Khan, S., Kizi, J. S. M., Fatima, T., & Malik, A. (2025). Exploring psychological recovery and coping mechanisms: post-flood mental health and resilience of women in Punjab, Pakistan. Discover Sustainability, 6(1), 107. https://doi.org/10.1007/s43621-025-00799-5
Alpaslan, C. M., & Mitroff, I. I. (2024). Spiritual versus Religious: A Natural Language Processing Perspective. Journal of Management, Spirituality & Religion, 21(1), 63–82. https://doi.org/10.51327/TUFP3116
Arthur, J., & Andoh-Quainoo, L. (2024). COVID-19 and Church Attendance Behavior Trends: Evidence from Ghanaian Pentecostal-Charismatic Churches. Spiritus: ORU Journal of Theology, 9(1). https://doi.org/10.31380/2573-6345.1348
Bodok-Mulderij, I., Schaap-Jonker, H., Klaassen-Dekker, A., Boselie, J., & Jacobs, N. (2023). The relation between religion/spirituality and mental health is mediated by self-compassion: Evidence from two longitudinal studies in the Dutch-speaking general population. Psychology of Religion and Spirituality, 15(3), 407–417. https://doi.org/10.1037/rel0000501
Bradshaw, M., Christopher, E., Qijuan, F., & Mueller, C. (2015). Listening to Religious Music and Mental Health in Later Life. The Gerontologist, 55(6), 961–971. https://doi.org/10.1093/geront/gnu020
Cassiani-Miranda, C. A., Cuadros-Cruz, A. K., Torres-Pinzón, H., Scoppetta, O., Pinzón-Tarrazona, J. H., López-Fuentes, W. Y., Paez, A., Cabanzo-Arenas, D. F., Ribero-Marulanda, S., & Llanes-Amaya, E. R. (2021). Validity of the Patient Health Questionnaire-9 (PHQ-9) for depression screening in adult primary care users in Bucaramanga, Colombia. Revista Colombiana de Psiquiatría (English Ed.), 50(1), 11–21. https://doi.org/10.1016/j.rcpeng.2019.09.002
Cha, L., Thai, J., True, M., Le, T., Ve’e, T., Soon, N. A., Bautista, R., & Tseng, W. (2024). A Community Assessment of Psychological Distress in Pacific Islanders Across San Francisco Bay Area Churches During the COVID-19 Pandemic. Journal of Racial and Ethnic Health Disparities, 11(1), 339–347. https://doi.org/10.1007/s40615-023-01522-8
Coulanges, F. de. (2024). The Ancient City a Study on the Religion, Laws, and Institutions of Greece and Rome. BoD – Books on Demand.
Craig, A., Rochat, T., Naicker, S., Mapanga, W., Mtintsilana, A., Dlamini, S. N., Ware, L. J., Du Toit, J., Draper, C. E., Richter, L., & Norris, S. A. (2022). The prevalence of probable depression and probable anxiety, and associations with adverse childhood experiences and socio-demographics: A national survey in South Africa. Frontiers in Public Health, 10. https://doi.org/10.3389/fpubh.2022.986531
Davenport, A. D., & McClintock, H. F. (2021). Let Go and Let God: A Study of Religiosity and Depressive Symptoms in the Black Church. Community Mental Health Journal, 57(7), 1340–1347. https://doi.org/10.1007/s10597-020-00757-7
Dietz, T. A., & Lorona, R. T. (2023). “Do not be anxious about anything”: Relationships between intrinsic religiosity, stigma of anxiety disorders, and treatment-seeking attitudes in a religiously affiliated university sample. Mental Health, Religion & Culture, 26(8), 815–826. https://doi.org/10.1080/13674676.2023.2283611
Dik, B. J., Daniels, D., & Alayan, A. J. (2024). Religion, Spirituality, and the Workplace: A Review and Critique. Annual Review of Organizational Psychology and Organizational Behavior, 11, 279–305. https://doi.org/10.1146/annurev-orgpsych-110721-041458
Du, L. J. (2024). The associations between religiosity and resilience when individuals are challenged by risk factors of suicide and mental illness. Frontiers in Public Health, 12, 1442248. https://doi.org/10.3389/fpubh.2024.1442248
Fernández-Niño, J. A., Bojorquez, I., Becerra-Arias, C., & Astudillo-Garcia, C. I. (2019). Religious affiliation and major depressive episode in older adults: A cross-sectional study in six low- and middle- income countries. BMC Public Health, 19(1), 460. https://doi.org/10.1186/s12889-019-6806-1
GBD 2019 Mental Disorders Collaborators. (2022). Global, Regional, and National Burden of 12 Mental Disorders in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. The Lancet Psychiatry, 9, 137-150. https://doi.org/10.1016/S2215-0366(21)00395-3
Hill, T. D., Ellison, C., & Hale, L. (2020). Religious attendance, depressive symptoms, and sleep disturbance in older Mexican Americans. Mental Health, Religion & Culture, 23(1), 24–37. https://doi.org/10.1080/13674676.2019.1710829
Himawan, K. K. (2020). The Single’s Struggle: Discovering Involuntary Singleness in Indonesia Through Gender and Religious Perspectives. 28(4), 379–389. https://doi.org/10.1177/1066480720950419
Hodge, D. R., Taylor, R. J., Chatters, L. M., & Boddie, S. C. (2022). Religious Involvement and DSM-IV Anxiety Disorders Among African-Americans. The Journal of Nervous and Mental Disease, 210(10), 784. https://doi.org/10.1097/NMD.0000000000001538
Holleman, A. (2023). The Resilience of Clergywomen?: Gender and the Relationship between Occupational Distress and Mental Health among Congregational Leaders. Journal for the Scientific Study of Religion -, 62(1), 89–107. https://doi.org/10.1111/jssr.12817
Hyde, J. S., & Mezulis, A. H. (2020). Gender Differences in Depression: Biological, Affective, Cognitive, and Sociocultural Factors. Harvard Review of Psychiatry, 28(1), 4. https://doi.org/10.1097/HRP.0000000000000230
Iheanacho, T., Nduanya, U. C., Slinkard, S., Ogidi, A. G., Patel, D., Itanyi, I. U., Naeem, F., Spiegelman, D., & Ezeanolue, E. E. (2021). Utilizing a church-based platform for mental health interventions: Exploring the role of the clergy and the treatment preference of women with depression. Global Mental Health, 8, e5. https://doi.org/10.1017/gmh.2021.4
Kaushal, A., Stafford, M., Cadar, D., & Richards, M. (2022). Bi-directional associations between religious attendance and mental health: Findings from a British birth cohort study. J Epidemiol Community Health, 76(2), 190–195. https://doi.org/10.1136/jech-2021-216943
Kim, K., Lim, H. J., Moon, E., & Moon, S. I. (2023). Influence of Optimism, Social Support, and Spirituality on COVID-19 Stress in Christian Church Community. Psychiatry Investigation, 20(2), 130–136. https://doi.org/10.30773/pi.2022.0243
Koenig, H. G., & Shohaib, S. S. A. (2019). Religiosity and mental health in Islam. In H. S. Moffic, J. Peteet, A. Z. Hankir, & R. Awaad (Eds.), Islamophobia and psychiatry: Recognition, prevention, and treatment (pp. 55–65). Springer Nature Switzerland AG. https://doi.org/10.1007/978-3-030-00512-2_5
Kuusi , T., Tervo-Niemelä, K. & Viertiö, S. Factors associated with psychological distress of workers in the Finnish Evangelical Lutheran Church. BMC Public Health 24, 875 (2024). https://doi.org/10.1186/s12889-024-18165-x
Lee, B.-H. J., Holleman, A., & Proeschold-Bell, R. J. (2024). Stability and shifts in the combined positive and negative mental health of clergy: A longitudinal latent class and latent transition analysis study of united methodist pastors before and after the onset of COVID-19. Social Science & Medicine, 344, 116651. https://doi.org/10.1016/j.socscimed.2024.116651
Lerman, S., Jung, M., Arredondo, E. M., Barnhart, J. M., Cai, J., Castañeda, S. F., Daviglus, M. L., Espinoza, R. A., Giachello, A. L., Molina, K. M., Perreira, K., Salgado, H., Wassertheil-Smoller, S., & Kaplan, R. C. (2018). Religiosity prevalence and its association with depression and anxiety symptoms among Hispanic/Latino adults. PLOS ONE, 13(2), e0185661. https://doi.org/10.1371/journal.pone.0185661
Lloyd, C. E. M. (2024). “Prayer Is Fine, but Don’t Then Quickly Move on, as If You’re Done and Dusted”: How Can the Evangelical Church Better Support Those with Mental Illness? Journal of Disability & Religion, 28(2), 110–131. https://doi.org/10.1080/23312521.2023.2173712
Lloyd, C. E. M., Mengistu, B. S., & Reid, G. (2022). “His Main Problem Was Not Being in a Relationship With God”: Perceptions of Depression, Help-Seeking, and Treatment in Evangelical Christianity. Frontiers in Psychology, 13, 831534. https://doi.org/10.3389/fpsyg.2022.831534
Lloyd, C. E. M., & Waller, R. M. (2020). Demon? Disorder? Or none of the above? A survey of the attitudes and experiences of evangelical Christians with mental distress. Mental Health, Religion & Culture, 23(8), 679–690. https://doi.org/10.1080/13674676.2019.1675148
Lucchetti, G., Koenig, H. G., & Lucchetti, A. L. G. (2021). Spirituality, religiousness, and mental health: A review of the current scientific evidence. World Journal of Clinical Cases, 9(26), 7620–7631. https://doi.org/10.12998/wjcc.v9.i26.7620
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Prof Kebogile Mokwena, Khomotso Maaga, Dr Oria Ramatsui, Dr Vukile Msizi Ngema , Ms Machaka Ravhengani

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.




