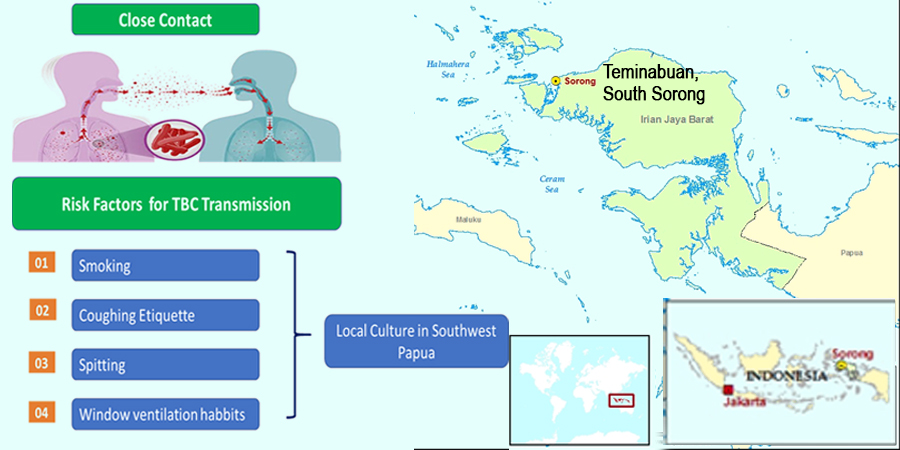
Local Culture and The Risk of Pulmonary Tuberculosis
A Case Study in Teminabuan Community Health Center, Indonesia
DOI:
https://doi.org/10.24252/diversity.v6i1.59052Keywords:
cough, mastication, pulmonary, smoking, tuberculosisAbstract
Pulmonary tuberculosis (TB) remains a persistent public health challenge globally, with Indonesia ranking among the highest burden countries. In regions such as Southwest Papua, the incidence of TB is strongly influenced by cultural practices and daily behavioral patterns, yet limited studies have explored this dimension. This study aimed to analyze behavioral factors related to pulmonary TB incidence in Teminabuan, Indonesia, focusing on ventilation practices, cough etiquette, sputum disposal, smoking, and betel nut chewing. A cross-sectional design was conducted from May to June 2024 involving 97 respondents, consisting of families and neighbors of TB patients, selected through purposive sampling. The majority of participants were indigenous Papuans (76.29%), with 44.33% consuming betel nut and 43.33% spitting indiscriminately. Bivariate analysis showed that poor ventilation, inadequate cough etiquette, and indiscriminate spitting were significantly associated with TB incidence (p < 0.05). Among these, indiscriminate spitting was the most influential factor (PR = 0.421; 95% CI: 0.194–0.648). Smoking showed no significant association, while betel nut chewing, often accompanied by spitting, was found to increase TB transmission risk. These findings underscore the urgent need for culturally sensitive interventions that address traditional practices, while promoting the principle of cleanliness as part of faith in Islam, thereby strengthening family health protection and TB control efforts.
Downloads
References
Abu-Ras, W., Aboul-Enein, B. H., Almoayad, F., Benajiba, N., & Dodge, E. (2024). Mosques and public health promotion: a scoping review of faith-driven health interventions. Health Education & Behavior, 51(5), 677-690. https://doi.org/10.1177/10901981241252800
Adeoye, B. D., Michael, T. O., & Agbana, R. D. (2024). Insights, beliefs, and myths surrounding tuberculosis among pulmonary patients with delayed healthcare access in a high-burden TB state in Nigeria–a qualitative inquiry. Frontiers in sociology, 9, 1378586. https://doi.org/10.3389/fsoc.2024.1378586
Alipanah, N., Jarlsberg, L., Miller, C., Linh, N. N., Falzon, D., Jaramillo, E., & Nahid, P. (2018). Adherence interventions and outcomes of tuberculosis treatment: A systematic review and meta-analysis of trials and observational studies. PLoS medicine, 15(7), e1002595. https://doi.org/10.1371/journal.pmed.1002595
Apatzidou D. A. (2022). The role of cigarette smoking in periodontal disease and treatment outcomes of dental implant therapy. Periodontology 2000, 90(1), 45–61. https://doi.org/10.1111/prd.12449
Balasubramnian, A., Francis, P. T., Leelamoni, K., Rakesh, P. S., & Lalu, J. S. (2022). Diagnostic and treatment delay among new pulmonary tuberculosis patients in Southern India: A cross-sectional study. Indian journal of public health, 66(Supplement), S60–S65. https://doi.org/10.4103/ijph.ijph_1079_22
Cao, X., Wang, Y., Chen, Y., Zhao, M., Liang, L., Yang, M., Li, J., Peng, M., Li, W., Yue, Y., Zhang, H., Li, C., & Shu, Z. (2023). Advances in traditional Chinese medicine for the treatment of chronic obstructive pulmonary disease. Journal of ethnopharmacology, 307, 116229. https://doi.org/10.1016/j.jep.2023.116229
Corrales, L., Rosell, R., Cardona, A. F., Martín, C., Zatarain-Barrón, Z. L., & Arrieta, O. (2020). Lung cancer in never smokers: The role of different risk factors other than tobacco smoking. Critical reviews in oncology/hematology, 148, 102895. https://doi.org/10.1016/j.critrevonc.2020.102895
Dickerson, D., Baldwin, J. A., Belcourt, A., Belone, L., Gittelsohn, J., Keawe’aimoku Kaholokula, J., Lowe, J., Patten, C. A., & Wallerstein, N. (2020). Encompassing cultural contexts within scientific research methodologies in the development of health promotion interventions. Prevention Science, 21(Suppl 1), 33-42. https://doi.org/10.1007/s11121-018-0926-1
Esmail, H., Macpherson, L., Coussens, A. K., & Houben, R. M. G. J. (2022). Mind the gap - Managing tuberculosis across the disease spectrum. EBioMedicine, 78, 103928. https://doi.org/10.1016/j.ebiom.2022.103928
Felgueiras, F., Mourão, Z., Moreira, A., & Gabriel, M. F. (2022). A systematic review of ventilation conditions and airborne particulate matter levels in urban offices. Indoor Air, 32(11), e13148. https://doi.org/10.1111/ina.13148
Fox, G. J., Redwood, L., Chang, V., & Ho, J. (2021). The effectiveness of individual and environmental infection control measures in reducing the transmission of Mycobacterium tuberculosis: a systematic review. Clinical Infectious Diseases, 72(1), 15-26. https://doi.org/10.1093/cid/ciaa719
Galvin, J., Tiberi, S., Akkerman, O., Kerstjens, H. A. M., Kunst, H., Kurhasani, X., Ambrosino, N., & Migliori, G. B. (2022). Pulmonary tuberculosis in intensive care setting, with a focus on the use of severity scores, a multinational collaborative systematic review. Pulmonology, 28(4), 297–309. https://doi.org/10.1016/j.pulmoe.2022.01.016
Gebeyehu, E. M., Mebratu, A., Atnafu, A., & Hagos, A. (2025). Process evaluation of Tuberculosis infection control and prevention practice at public health facilities in Tegede district, Northwest Ethiopia: Facility-based cross-sectional design. PloS one, 20(2), e0314514. https://doi.org/10.1371/journal.pone.0314514
Iskandar, D., Suwantika, A. A., Pradipta, I. S., Postma, M. J., & van Boven, J. F. M. (2023). Clinical and economic burden of drug-susceptible tuberculosis in Indonesia: national trends 2017-19. The Lancet Global Health, 11(1), e117–e125. https://doi.org/10.1016/S2214-109X(22)00455-7
Islam, M. S., Chughtai, A. A., Banu, S., & Seale, H. (2021). Context matters: Examining the factors impacting the implementation of tuberculosis infection prevention and control guidelines in health settings in seven high tuberculosis burden countries. Journal of Infection and Public Health, 14(5), 588-597. https://doi.org/10.1016/j.jiph.2021.01.014
Kak, N., Chakraborty, K., Sadaphal, S., AlMossawi, H. J., Calnan, M., & Vikarunnessa, B. (2020). Strategic priorities for TB control in Bangladesh, Indonesia, and the Philippines - comparative analysis of national TB prevalence surveys. BMC Public Health, 20(1), 560. https://doi.org/10.1186/s12889-020-08675-9
Kumawat, A., Chakraborti, A., Kumar, S., Sonigra, M., Bhatnagar, A., Kumar, A., & Chopra, K. K. (2023). Study of factors leading to treatment delay in new sputum positive pulmonary tuberculosis patients and its impact on sputum conversion. Tropical Doctor, 53(2), 227-232. https://doi.org/10.1177/00494755221137118
Lestari, B. W., McAllister, S., Hadisoemarto, P. F., Afifah, N., Jani, I. D., Murray, M., van Crevel, R., Hill, P. C., & Alisjahbana, B. (2020). Patient pathways and delays to diagnosis and treatment of tuberculosis in an urban setting in Indonesia. The Lancet Regional Health - Western Pacific, 5, 100059. https://doi.org/10.1016/j.lanwpc.2020.100059
Malik, S. G., Oktavianthi, S., Wahlqvist, M. L., Asih, P. B. S., Harahap, A., Satyagraha, A. W., & Syafruddin, D. (2020). Non-nutritional anemia: Malaria, thalassemia, G6PD deficiency and tuberculosis in Indonesia. Asia Pacific Journal of Clinical Nutrition, 29. https://doi.org/10.6133/apjcn.202012_29(S1).04
Manghani, P., Prasad, N., Khatri, N., Paulino-Ramirez, R., Gokhale, S., Islam, K. M. M., Majumdar, P., Hoang, T., & Denny, H. (2024). Betel Quid Use and Tuberculosis Transmission: A Neglected Focus Area for Tuberculosis Control in Low- and Middle-Income Countries. Open Forum Infectious Diseases, 11(11). https://doi.org/10.1093/ofid/ofae577
Marahatta, S. B., Yadav, R. K., Giri, D., Lama, S., Rijal, K. R., Mishra, S. R., Shrestha, A., Bhattrai, P. R., Mahato, R. K., & Adhikari, B. (2020). Barriers in the access, diagnosis and treatment completion for tuberculosis patients in central and western Nepal: A qualitative study among patients, community members and health care workers. PLOS ONE, 15(1), e0227293. https://doi.org/10.1371/journal.pone.0227293
McLaren, H., Patmisari, E., Hamiduzzaman, M., Jones, M., & Taylor, R. (2021). Respect for religiosity: review of faith integration in health and wellbeing interventions with Muslim minorities. Religions, 12(9), 692. https://doi.org/10.3390/rel12090692
Mohidem, N. A., & Hashim, Z. (2023). Integrating Environment with Health: An Islamic Perspective. Social Sciences, 12(6), 321. https://doi.org/10.3390/socsci12060321
Irfan, B., Khleif, A., Badarneh, J., Abutaqa, J., Allam, A., Kweis, S., & Padela, A. (2025). Considering Islamic Frameworks to Infectious Disease Prevention. In Open Forum Infectious Diseases (p. ofaf011). https://doi.org/10.1093/ofid/ofaf011
Noora, C., Bandoh, D., Nuoh, R., Sarfo, B., Nyarko, K., & Kenu, E. (2020). Evaluation of timeliness of treatment initiation among smear positive pulmonary tuberculosis patients in Brong Ahafo Region, Ghana, 2015. Ghana Medical Journal, 54(2), 73-82. https://doi.org/10.4314/gmj.v54i2s.12
Obore, N., Kawuki, J., Guan, J., Papabathini, S. S., & Wang, L. (2020). Association between indoor air pollution, tobacco smoke and tuberculosis: an updated systematic review and meta-analysis. Public health, 187, 24-35. https://doi.org/10.1016/j.puhe.2020.07.031
Onmek, N., Kongcharoen, J., Singtong, A., Penjumrus, A., & Junnoo, S. (2020). Environmental factors and ventilation affect concentrations of microorganisms in hospital wards of Southern Thailand. Journal of Environmental and Public Health, 2020(1), 7292198. https://doi.org/10.1155/2020/7292198
Paleckyte, A., Dissanayake, O., Mpagama, S., Lipman, M. C., & McHugh, T. D. (2021). Reducing the risk of tuberculosis transmission for HCWs in high incidence settings. Antimicrobial Resistance & Infection Control, 10(1), 106. https://doi.org/10.1186/s13756-021-00975-y
Pele, M., Herawati, T., & Yona, S. (2021). Factors Influencing Transmission of Tuberculosis in Ngeu Nata Culture among Ngada Community in Kupang, East Nusa Tenggara, Indonesia: Cross Sectional Study. Journal of Public Health Research, 10(1_suppl). https://doi.org/10.4081/jphr.2021.2335
Piwko, A. M. (2021). Islam and the COVID-19 pandemic: Between religious practice and health protection. Journal of religion and health, 60(5), 3291-3308. https://doi.org/10.1007/s10943-021-01346-y
Pradipta, I. S., Idrus, L. R., Probandari, A., Puspitasari, I. M., Santoso, P., Alffenaar, J. W. C., & Hak, E. (2022). Barriers to optimal tuberculosis treatment services at community health centers: a qualitative study from a high prevalent tuberculosis country. Frontiers in pharmacology, 13, 857783. https://doi.org/10.3389/fphar.2022.857783
Quan, Z., Xu, J., Li, M., Cheng, C., Mijiti, P., Jiang, Q., Takiff, H., Ren, Z., & Gao, Q. (2024). Transmission of tuberculosis in rural Henan, China: a prospective population-based genomic spatial epidemiological study. Emerging microbes & infections, 13(1), 2399273. https://doi.org/10.1080/22221751.2024.2399273
Rai, S., Singh, D. K., & Kumar, A. (2021). Microbial, environmental and anthropogenic factors influencing the indoor microbiome of the built environment. Journal of Basic Microbiology, 61(4), 267-292. https://doi.org/10.1002/jobm.202000575
Shafique, S., Bhattacharyya, D. S., Nowrin, I., Sultana, F., Islam, M. R., Dutta, G. K., Del Barrio, M. O., & Reidpath, D. D. (2024). Effective community-based interventions to prevent and control infectious diseases in urban informal settlements in low-and middle-income countries: a systematic review. Systematic Reviews, 13(1), 253. https://doi.org/10.1186/s13643-024-02651-9
Shah, H. D., Nazli Khatib, M., Syed, Z. Q., Gaidhane, A. M., Yasobant, S., Narkhede, K., Bhavsar, P., Patel, J., Sinha, A., Puwar, T., Saha, S., & Saxena, D. (2022). Gaps and Interventions across the Diagnostic Care Cascade of TB Patients at the Level of Patient, Community and Health System: A Qualitative Review of the Literature. Tropical Medicine and Infectious Disease, 7(7), 136. https://doi.org/10.3390/tropicalmed7070136
Tamara, L., Kartasasmita, C. B., Alam, A., & Gurnida, D. A. (2022). Effects of Vitamin D supplementation on resolution of fever and cough in children with pulmonary tuberculosis: A randomized double-blind controlled trial in Indonesia. Journal of global health, 12, 04015. https://doi.org/10.7189/jogh.12.04015
Tewatia, P., Kaushik, R. M., Kaushik, R., & Kumar, S. (2020). Tobacco smoking as a risk factor for tuberculous pleural effusion: A case-control study. Global health, epidemiology and genomics, 5, e1. https://doi.org/10.1017/gheg.2020.1
Trajman, A., Campbell, J. R., Kunor, T., Ruslami, R., Amanullah, F., Behr, M. A., & Menzies, D. (2025). Tuberculosis. Lancet (London, England), 405(10481), 850–866. https://doi.org/10.1016/S0140-6736(24)02479-6
World Health Organization. (2022). Tuberculosis deaths and disease increase during the COVID-19 pandemic. https://www.who.int/news/item/27-10-2022-tuberculosis-deaths-and-disease-increase-during-the-covid-19-pandemic
Yablonskii, P. K., Kudriashov, G. G., & Avetisyan, A. O. (2019). Surgical resection in the treatment of pulmonary tuberculosis. Thorac Surg Clin, 29(1), 37-46. https://doi.org/10.1016/j.thorsurg.2018.09.003
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Ishaq Iskandar, Imelda Naolin, Arlin Adam, Harun Iskandar, yamsuri Syakri

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.




